Press release -
GEHWOL Diabetes Report 2021-2022: Advise diabetics, protect their feet!
Four out of five foot amputations in diabetics are preventable. This is shown by study-based estimates. (1) One prerequisite among others is: Risk awareness! And this is currently in short supply, according to the latest GEHWOL Diabetes Report. In other words: there is room for improvement in educating patients. (2) One third of diabetics are not aware that their feet need special care. The feet often go unno- ticed at check-ups, and recommended measures for identifying patients at risk are not always used at examinations. Generally, podological care at first diagnosis of diabetes could help to improve primary preventive care. 86% of doctors say this. Podological foot care is usually only recommended if there is also a prescription entitlement. On the other hand, doctors often fail to recommend podological care if patients have to bear the costs themselves.
The number of people affected by diabetes is steadily increasing. Currently, about 8 mil- lion people in Germany have type 2 diabetes. 32,000 children and adolescents and 341,000 adults have type 1 diabetes. It seems realistic to assume that about 11.5 million people in Germany will have type 2 diabetes by 2040. (3) Diabetes is associated with risks for consequential damage. Diabetic foot syndrome, or DFS for short, is a particularly serious complication. The clinical picture usually develops after many years of diabetes. It is characterized by complex processes. The simultaneous presence of diabetic nerve damage (polyneuropathy), diabetic vascular insufficiency (macro- and microangiopathy) and a weakened immune system plays an important role. Poorly healing skin lesions such as xerosis (dry skin) or callus (compact, hardened, excess callus) that develop un- der these conditions can develop into foot wounds (ulcers) and eventually into severe inflammatory tissue defects (necrosis). In the worst case, such processes lead to a com- plete or partial foot amputation. Diabetic patients still account for about two thirds of all amputations. The German Health Report Diabetes 2021 mentions 40,000 to 50,000 amputations per year; such amputations are often performed too early or unnecessarily in people with diabetes. Four out of five amputations would be avoidable with timely preventive care and appropriate risk management, according to a study. (1)
Timely prevention still has gaps
Prevention also involves the affected persons themselves as well as their relatives: For example, one should be proactive in foot health with preventive measures such as wear- ing the right footwear, inspecting your feet daily, and practicing intensive foot care. Risk awareness and patient behaviour have the greatest impact on outcomes when it comes to preventing foot complications. According to the current GEHWOL Diabetes Report, there is absolute agreement on this among doctors.
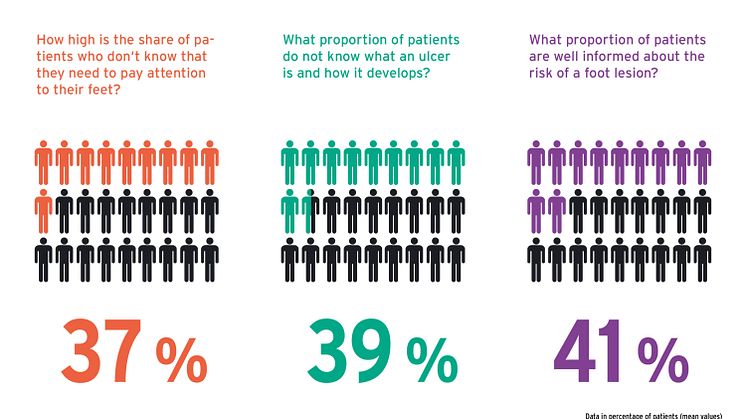
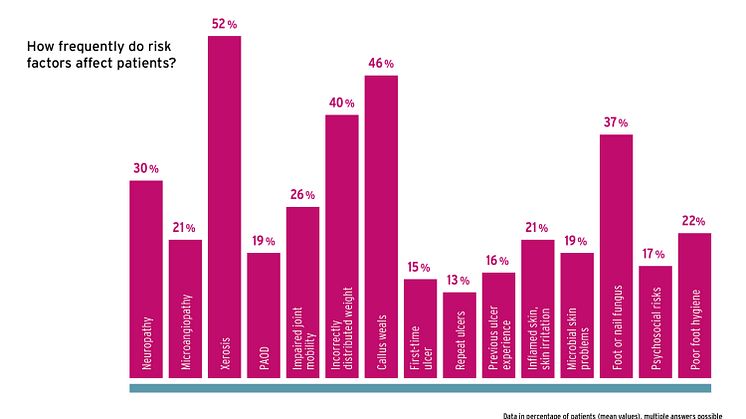
However, there is a constant lack of risk awareness and preventive behaviour among patients - even though 23% of those affected are considered to be at risk of DFS. This is also shown by the current GEHWOL Diabetes Report, which comes out every two years. Risk factors such as neuropathy (30%), microangiopathy (21%), macroangiopathy (19%), dry skin (52%), calluses (46%), pressure and weight-bearing dysfunctions (40%), limited joint mobility (26%) and foot or nail fungus (37%) are common. According to the doctors interviewed in the report, many affected persons are still unaware of the dangers posed by these symptoms. 37% of patients are not aware that they need to take care of their feet (comparison to 2017: 38%; 2019: 33%). 39% of those affected do not know what an ulcer is or how it develops (2017: 56%, 2019: 39%). Overall, less than half of all diabetics are well informed and aware of the risks of a foot lesion, according to their doctors. In view of this data from the new GEHWOL Diabetes Report, it is not surprising that only 21% of doctors describe their patients as having good awareness, particularly when it comes to foot care. 14% and more give their patients a grade of 5 = insufficient.
Concrete recommendations for action on preventive care
The IWGDF International Working Group on Diabetic Feet [Internationale Arbeitsge- meinschaft Diabetischer Fuß] has adopted a number of counselling recommendations for patient consultations in its prevention guidelines (4). They aim to improve risk aware- ness and support healthcare professionals in improving care for diabetics, especially those who are at risk of developing ulcers. In practice, however, it is evident that these recommendations are only partially implemented - and not for all patients. Only 57% of doctors generally inform all diabetics about early preventive care, while the rest do so only if there is an identifiable ulcer risk.
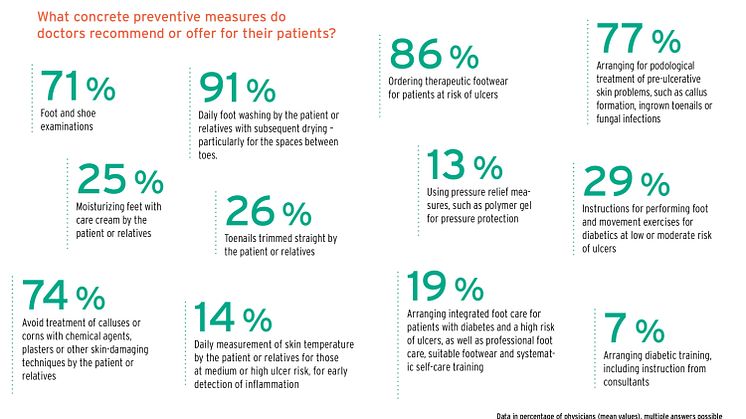
According to the guideline, the provision of integrated foot care for patients with diabetes and a high risk of ulcers is a cornerstone of preventive care, including professional foot care, appropriate footwear and systematic education on self-care. However, according to the Diabetes Report, only 19% of practitioners follow this recommendation. Other rec- ommendations are also rarely taken into account. Thus, the feet should be treated with care cream by patients or caregivers. Only one-quarter of doctors recommend this. Toe- nails should be cut straight - again, only one-quarter of doctors recommend this. Only 14% of doctors specifically recommend or order that patients - at least those with medium ulcer risk or higher - should measure their skin temperature in order to recognize inflam- mation in time. Only 13% point out pressure relief measures such as using polymer gel pressure relief cushions. 29% of doctors give instructions on how to perform physical exercises. Foot inspection, hygiene and consistent pressure relief with special orthopae- dic footwear is generally considered very important for prevention. Accordingly, these measures are well established in medical advice. 71% of doctors recommend examining the feet and shoes. 91% point out the need to wash and dry the feet daily, especially between the toes. 86% order custom therapeutic shoes for patients at risk of ulcers.
Early podological care is desirable
Regular podiatric treatments are an essential part of diabetes risk management. How- ever, not even half of the patients have their feet checked at a podiatry practice. This might be partly due to the fact that medical prescriptions are only issued when there are positive findings, such as evident skin problems, but not immediately at first diagnosis. Accordingly, 39% of doctors currently recommend a podiatric examination only if there is a prescription entitlement. Nonetheless, the remaining 61% also advise this if the pa- tient has to bear the costs themselves. There is even more reluctance to order biome- chanical examinations by an orthopaedic shoemaker to identify pressure load problems. Only 42% of doctors specifically order this even if there is no prescription entitlement; the rest do so only if the patient is entitled to a prescription for it.
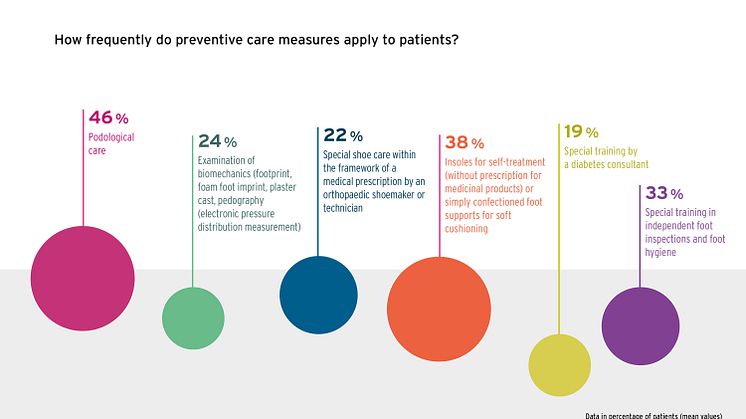
Only 24% of patients currently have their gait biomechanically examined, e.g. by taking a footprint, foot foam, plaster cast or electronic pressure distribution measurement (pedography). Only 22% receive special shoe care as part of a medical aid prescription, according to the figures contained in the GEHWOL Diabetes Report.
Education should not be left solely to medical professionals
Surveyed doctors are 100% aware of their advisory responsibility, the GEHWOL Diabe- tes Report shows. However, diabetic care is usually an interdisciplinary matter. Doctors therefore also see other professional groups as being responsible. These include podi- atrists, diabetes counsellors and specialist staff in pharmacies. The example of care products used in foot care at home can be used to illustrate the benefits of network coun- selling. It is true that doctors are generally rather reluctant to recommend using cream on the feet as a specific course of action. Nevertheless, they have a clear idea of what a care product must achieve. The focus is on effectiveness, according to 89% of doctors. Most doctors inform their patients that the products should contain urea at varying con- centrations, such as 10% for dry skin or more for excess callus.
A recent study also confirms that it is beneficial to use urea-containing formulations in different dosages depending on the area of application. (5) However, it also concludes that more evidence is needed regarding the use of urea for the prevention of diabetic foot complications - an assessment shared by 43% of physicians. This is especially true since the desired efficacy depends not only on urea, but on the overall formulation which can provide further useful effects for diabetics. For example, 59% of doctors recommend paying attention to formulations that have a positive influence on the skin microcircula- tion, i.e. the skin's blood circulation. Blood circulation is reduced in many diabetics, as confirmed by the GEHWOL Diabetes Report. Lack of blood circulation in the skin is a typical cause of dry, brittle skin due to diabetes. Specialist staff in pharmacies and podi- atry practices can help patients choose suitable care products that positively influence the skin's circulation.
Opportunities for optimizing preventive care
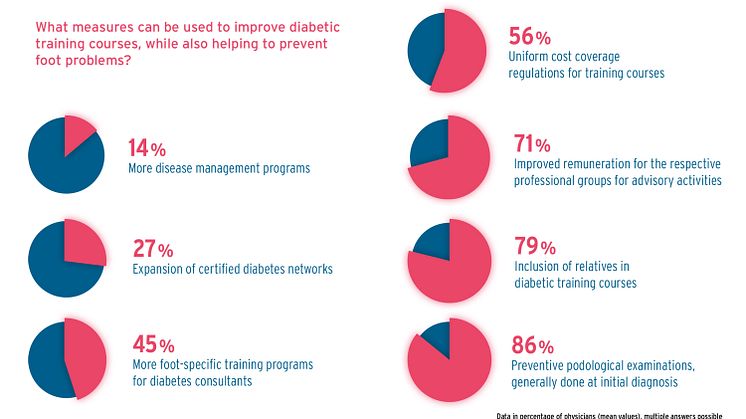
Strengthening interdisciplinary treatment and counselling has potential for making pro- gress in the primary prevention of foot problems. This conclusion is consistent in view of the importance that doctors attribute to podological treatment in particular, but also to education by trained diabetes counsellors. Podiatric screening in general at initial diag- nosis is an approach that most interviewed doctors support to strengthen prevention. 86% of doctors hold this opinion. Better remuneration of professionals for advisory activ- ities could also be helpful, according to 71% of respondents. For training by diabetes counsellors, cost reimbursements should be regulated uniformly (56%) and more foot- specific further training should also be offered for service providers (45%). There is a definite need for this - according to 61% of doctors, instruction in injury-free foot care is often neglected in training courses. In this context, it could also be helpful to involve caregivers. On the patient's side, however, it can be observed that only about one-third of diabetics actually receive such training.
Optimization opportunities in diagnosing risks
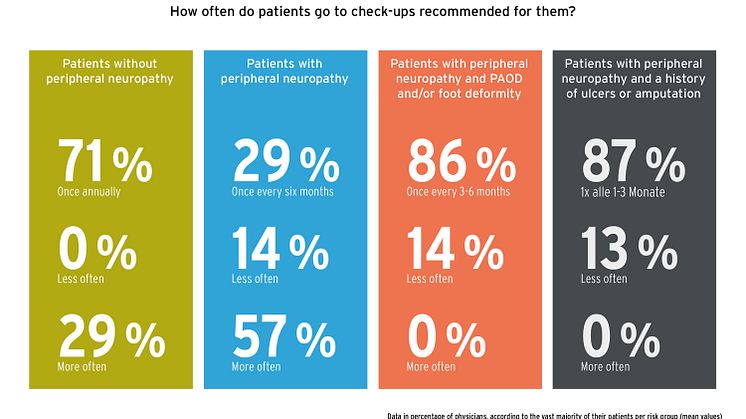
Even the best counselling intentions are useless if patients do not take advantage of available preventive care services. This concerns not only network measures such as podiatry consultations, or group or individual diabetes training courses. There are deficits even in the perception of medical check-ups. A risk-adapted examination interval with defined contents is recommended for diagnostics. (6) In patients without neuropathy, the examination should take place once a year, in patients with neuropathy once every six months; in neuropathy and angiopathy (PAOD) or foot deformity, it should be once every three to six months. Patients with a history of neuropathy and ulcers or amputation should be examined once every one to three months. A dilemma becomes apparent here. The lowest-risk patients largely comply with the recommended intervals, according to 71% of doctors. 29% even confirm more frequent examinations. However, up to 14% of doctors report that high-risk patients in particular come in for visits less often than recommended.
Not all examination measures take place according to recommendations
This is problematic because relevant risk diagnostics cannot be carried out at appropriate intervals in these patients. This includes the specific medical history, examinations of skin status, muscles, existing foot deformities and mobility, skin temperature, checking the shoes, examination of pressure sensitivity, vibration sensation as well as foot pulses. The good news: Most medical practices carry out these measures during examinations.
However, 11% and 9% respectively say that they do not measure skin temperature and check patients' shoes.
Nonetheless, conditions are certainly not optimal. For practically all measures, a more or less large proportion of doctors state that the respective examination is not carried out - as recommended - at every check-up appointment. For example, 43% of doctors do not measure pressure sensitivity with a special probe (10-g monofilament) at every ex- amination; 52% do not measure vibration sensation (using a Rydell-Seiffer tuning fork), and 45% do not measure foot pulses (posterior tibial artery, dorsalis pedis artery) bilat- erally at every appointment. According to the clinical recommendations of the German Diabetes Society, these measures, among others, should be part of every foot examina- tion.
Safety diagnostics even with palpable foot pulses
Foot pulses are a possible indicator for the presence of angiopathy (PAOD). However, clinical recommendations also point out that the presence of palpable foot pulses does not exclude PAOD. Further examinations are recommended for this reason - such as doing an extended pulse status (popliteal artery, femoral artery) or checking index values at the ankle and arm (ABI) or at the toes and arm (TBI). 13% of doctors always follow this recommendation, even if foot pulses are palpable, while the majority (87%) refrain from further diagnostics in this case. However 72% of doctors immediately carry out ap- propriate measures to determine an extended pulse status if no foot pulses are palpable. 28% immediately do a referral to a specialist, for example, for imaging procedures (ul- trasound, MR/CT angiography).
Short version (lead): 830 characters | Long version: 14,170 characters
Reprint free | copy requested
Sources:
- Mohamad A. et al. Population-based secular trends in lower extremity amputation for diabetes and peripheral artery disease. CMAJ Sep 2019; 191 (35): E955-E961; DOI: 10.1503/cmaj.190134
- GEHWOL Diabetes Report 2021-2022. Structured standardized written survey with n = 2,793 patients via n = 107 doctors. Survey and evaluation by IDS Germany and INSIGHT Health June to August 2021. On the internet incl. download: https://www.gehwol.de/Aktuelle...
- German Health Report Diabetes 2021. German Diabetes Association (DDG [Deutsche Diabetes Gesellschaft]) and diabetesDE - German Diabetes Aid Society [Deutsche Diabetes-Hilfe]. Kirchheim, Mainz: 2020.
- IWGDF Guidelines on the prevention and management of diabetic foot disease, 2019 version. Online: https://iwgdfguidelines.org/
- Bowen G. et al. Optimal emollient treatment and prevention of diabetic foot compli- cations. The Diabetic Foot Journal 2021; 24 (1): 40 – 45.
- Practice recommendations of the German Diabetes Association. Updated version of 2020, Diabetology 2020; 15: S206–S215; DOI 10.1055/a-1194-1790
Key Findings:
- 37% of patients are not aware that their feet need special care.
- 46% of patients receive podological care.
- 22% of patients have specially fitted shoes.
- 33% of patients receive training in foot inspections and hygiene.
- 14% of patients have inadequate footwear.
- 57% of doctors educate all patients about foot inspections and care, while 43% merely educate patients who have a recognizable ulcer risk / high-risk patients.
- 39% of doctors only recommend podological treatment if there is a prescription entitlement and the patient can be issued a prescription.
- 19% of physicians arrange integrated foot care, including professional foot care, appropriate shoe care and systematic education.
- 86% of physicians generally regard podological screenings at initial diagnosis as an opportunity to improve primary preventive care.
- 79% of physicians see opportunities for improving preventive care training for care- givers of diabetics.
- According to up to 14% of doctors, high-risk patients do not pay attention to the recommended examination intervals - even when they have a history of ulcers or amputations.
- 81% of doctors check shoes, but 47% do not do so at every examination.
- 13% of physicians perform additional measures to check the pulse status to be on the safe side, even when the foot pulses are palpable.
- 91% of physicians strongly recommend getting a second opinion before an amputation.
Related links
Topics
Categories
With its two brands, GEHWOL and GERLACH TECHNIK, Eduard Gerlach GmbH is one of the most popular complete providers of foot care products and technology. Its full product range includes products with various pharmaceutical forms, galenics and active substance formulations and for different skin types and skin problems. These products are available exclusively from foot care practices, cosmetics institutes and pharmacies.